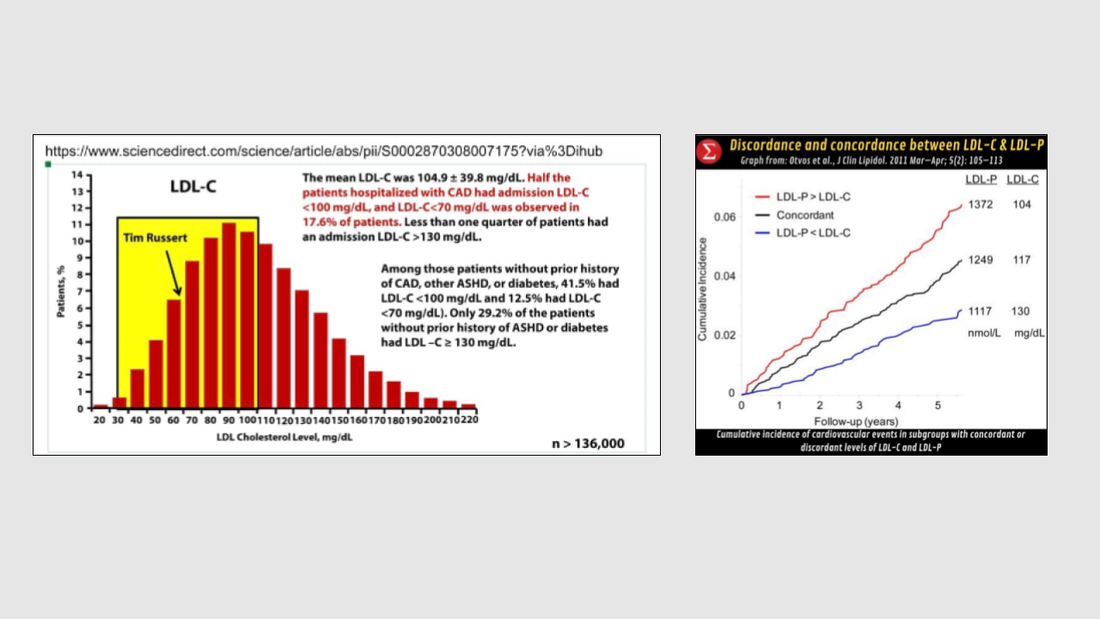
Since 50% of the people who had a heart attack had normal LDL-C (“bad cholesterol”) results (Fig. 1), the real problem lies in either not identifying all the metrics that really matter or the LDL cholesterol needs to be lowered further. While LDL-C, HDL-C, Triglycerides, HbA1c, BMI, blood pressure, etc. are important markers, there are others that have been shown to be as important in diagnosing the state of one’s heart health. Getting a comprehensive heart health assessment done across blood, body composition and physiological markers provides a more holistic view of the heart's functioning. I want to focus on one specific marker that is a much better indicator of heart health, especially for folks who have some other comorbidity, such as pre-diabetes, diabetes, hyperinsulinemia, etc: Your ApoB measurement, which is essentially the total number of LDL particles (or LDL-P) carrying that cholesterol. LDL-C is a good measure of atherosclerosis (cardiovascular degeneration) only as long as the cholesterol to triglycerides ratio in each LDL particle is at the typical distribution. The moment that changes (typically due to some sort of comorbidity), LDL-C and LDL-P become discordant and in such situations, LDL-P is the better indicator of cardiovascular disease. Check out Fig. 2 to see the long term risk when they become discordant, specifically when LDL-P > LDL-C. Extensive work done by the South Asian Heart Center, a non-profit organization, requires that ApoB levels be less than 50 mg/dL for South Asians in their blood tests, while the Lipid Association of India recommends ApoB levels less than 50 mg/dl, 65 mg/dl and 80 mg/dl for those at extreme risk, very high risk and high risk of cardiovascular diseases respectively, rather than the 46 - 174 mg/dL that is used in the few cases it is even measured.
Bottomline: Make sure to ask your doctor to include LDL-P (or ApoB) in your next blood test and get your Lp(a) tested for as well (your genetic risk component which cannot be changed through lifestyle alone). If you are interested in getting a very focused heart health assessment done with the parameters and ranges optimized for you, drop me a note. The GeneClinicX Heart Health Assessment test includes blood, body composition and physiological parameter measurements and is done at your home. You get a 30-minute session with a counselor, where we will explain your results and answer any questions you may have. This test is only available in India but we will be launching a test in the US shortly.

14 comments
Mandar Gadre: ApoB is better than LDL to assess CVD risk, yes. Also, when we look at overall risk factors & associated markers, a bigger picture emerges. Insulin Resistance & Triglycerides are bigger than ApoB, LDL. Type-2 Diabetes and Metabolic Syndrome are more important than genetic history. Thus, we need to focus on the TG:HDL ratio which is the strongest predictive factor for heart diseases (lower than 2 is good. Lower the better)
Supporting material:
1) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2664115/ (TG:HDL ratio showed the strongest association with extent of heart disease)
2) https://www.nature.com/articles/s41598-021-00020-3 (TG:HDL ratio & CTA risk score worsened despite increased use of lipid-lowering drugs and reduction in LDL-C)
3) https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/647239 (Low TG:HDL = low risk of heart disease even when LDL is high)
Thus, I would focus on TG:HDL ratio as the strongest predictive marker for heart disease risk. And work on lowering insulin resistance. Also, this may be interesting: https://www.bmj.com/content/371/bmj.m4266 Study with 100K+ patients, mean follow-up 9+ years
The study concluded that BOTH low & high levels of LDL-C were associated with an increased risk of all-cause mortality and the lowest risk of all-cause mortality was found at an LDL-C of 140 mg/dL.
Nickhil Jakatdar: Thanks. For South Asians, a metric that seems to be more relevant is the non-HDL-C to Apo(B) ratio. This was based on the data collected exclusively on South Asians for the last 10 years and unsurprisingly the race-specific insights showed up in the data very nicely. While many of the markers were the usual age and BMI, this marker showed up third in terms of impact. This paper from Denmark has a number of fundamental issues because of which it was rejected by this journal after peer review. This is what makes keeping up with the latest science quite challenging ie. papers get a pre-review publication giving the sense that it is acceptable science. If you want to take a look at the holes pointed out in this publication check out: https://www.bmj.com/sites/default/files/attachments/bmj-article/pre-pub-history/first_decision_19.8.20_1.pdf
Mandar Gadre: Thanks for sharing. Trying to understand the below: (for the paper about Risk in South Asians, and non-HDL: ApoB ratio). I see that p-values for all lipid markers show no statistical significance. How does that square with non-HDL: ApoB ratio being the strongest predictor? Also, p-value for Birthplace also shows no statistical significance. So how do we apply it specifically to South Asians? Genuinely curious. Am I missing something? For the Danish paper, will need to take a look. Thanks for sharing the reviewer’s comments. One thing I’m wary of about the focus on LDL – and prescriptions of LDL-lowering statins – is that these drugs worsen insulin resistance, which is a bigger associated risk factor. I’ll admit that I’m biased towards nutrition-exercise-lifestyle interventions before (and instead of) medications. But I don’t think that’s a bad thing.
Nickhil Jakatdar: I am in the same bucket. I too believe in the power of nutrition and exercise as you may have probably seen in my last post a week back. However statins have a role to play, typically in stabilizing plaque. I would still rather reduce my numbers through lifestyle changes but plaque stabilization for those that already have significant plaque cannot be done through lifestyle. On your point about statins increasing insulin resistance, certain statins like atorvastatin are absolutely known to do that. However, I was able to bring my HbA1c down to counter the statin through lifestyle changes.
Shashi Karpur: Nickhil – Please add me to the mailing list for your US launch? Thanks.
Nickhil Jakatdar: I will keep you posted.
Ashish Chitale: Incredible work. I will surely be getting the test done, start paying close attention to these markers and will start talking about it with friends and colleagues. Thank you for writing these potentially life-saving blogs.
Nickhil Jakatdar: Thank you for spreading the word.
Nish Bhutani: Thanks Nickhil. Do you have a link handy to this test? "GeneClinicX Heart Health Assessment test "
Nickhil Jakatdar: Nish I’ll have someone send you the HHA brochure. Pls message me your email address or whatsapp number to send it to.
Chetan Channa: Hi Nickhil. Who can I reach out to for the test. Turned 40 this year and want to get my baselines measured as I have a family history of cardiac diseases on both the sides. Thanks.
Nickhil Jakatdar: Chetan I’ll have my team connect with you. Pls let me know if the WhatsApp info I have is still the same. Glad you are staying on top of your health.